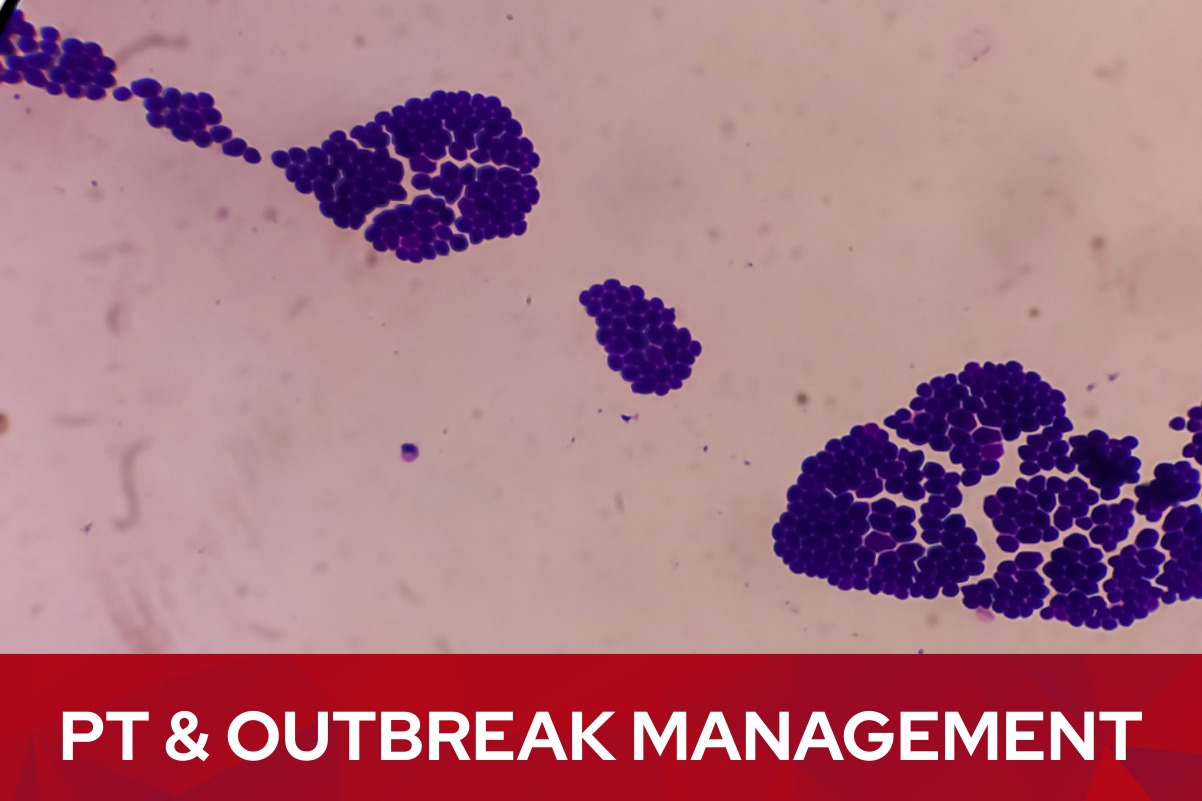
Mastering Your Lab's Quality
Ten Steps to Successful Proficiency Testing
As we move into the busy first quarter of the year, ensuring that your laboratory’s quality systems are running smoothly is more important than ever. Having a clear, organized approach can make every testing event seamless. To help your team achieve the best possible results, we are highlighting our latest resource, the “Ten Steps to Successful Proficiency Testing” guide (ppt). Whether you are a seasoned lab professional or new to the process, following these ten essential steps can help prevent common errors and ensure regulatory compliance.

Phase 1: Preparation and Planning
Success begins long before the samples arrive. First, ensure your enrollment confirmation packet is reviewed and that key information, like the shipping schedule and contact numbers, is posted in a prominent, accessible place for all staff. Regularly review our shipping schedule to confirm that staff will be available for receipt and testing and that all necessary supplies, reagents, and preventive maintenance are up to date.
Phase 2: Handling and Routine Testing
When PT samples arrive, they should be documented and opened immediately to check for any damage or missing items. Utilizing a dedicated PT Tracking Sheet helps confirm proper storage and handling from the moment of receipt.
Prior to testing, schedule your personnel on a rotating basis to ensure all staff who perform patient testing also participate in PT. On the day of testing, perform your standard instrument checks and quality control just as you would for patient samples. During the testing of PT samples, it is vital to handle them in the same routine manner as patient specimens—do not refer them to other labs or compare results with other locations.
Phase 3: Resulting and Submission
Accurate results entry requires verifying sample IDs, units, and decimal places as requested in the instructions. Before final submission, verify that your instrument and method information is correct in PT Central and ensure the attestation statement is signed by both testing personnel and the laboratory director. Finally, submit your proficiency testing results before the due date online and save a copy of your Data Submission Report for your records.
Phase 4: Evaluation and Follow-Up
Once the evaluation report is returned, review it thoroughly, paying close attention to any scores less than 100% or non-consensus results. The final step is post-event follow-up, which involves investigating and documenting any necessary corrective actions and performing self-evaluations for ungraded results. Remember to maintain all PT records for at least two years (and five years for blood bank records).
Resources for Your Team
For a detailed breakdown of these steps, including visual guides and troubleshooting forms, you can view the full Ten Steps to Successful Proficiency Testing PowerPoint presentation on our Resources webpage at https://wslhpt.org/resources/.
If you have questions or need assistance with your next testing event, our customer service team is available at (800) 462-5261 or via email at ptservice@slh.wisc.edu.